What is Gum Disease?
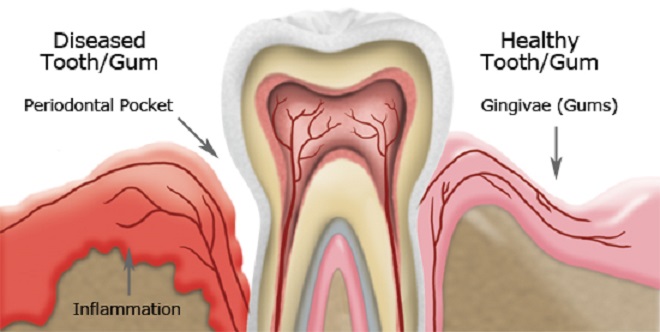
Certainly you’ve heard terms such as: Gum Disease, Plaque, Calculus, Gingivitis, Periodontitis, Periodontal Disease, Tartar. But what do these terms mean? Gum Disease (also known as Periodontal Disease) starts when plaque and tartar (calculus) are allowed to accumulate at the base of your teeth. The bacteria in the plaque leads to an infection in the gums (gingiva) called Gingivitis. If left untreated, the infection spreads to the tissue and bone that holds your teeth in place, a condition called Periodontitis. Because gum disease is usually painless, you may not know you have it.
Periodontal diseases range from simple gum inflammation to serious disease that results in major damage to the gums (soft tissue) and bone that support the teeth. It is a major cause of tooth loss in adults.
Mild Gum Disease (Gingivitis)
The longer plaque and tartar are on teeth, the more harmful they become. The bacteria cause inflammation of the gums that is called gingivitis. In gingivitis, the gums become red, swollen and can bleed easily. Gingivitis is a mild form of gum disease that can usually be reversed with daily brushing and flossing, and regular cleaning by a registered dental hygienist. This form of gum disease does not include any loss of bone and tissue that hold teeth in place.
Advanced Gum Disease (Periodontitis)
When gingivitis is not treated, it can advance to periodontitis (which means inflammation around the tooth). In periodontitis, gums pull away from the teeth and form spaces (called pockets) that become infected. The body’s immune system fights the bacteria as the plaque spreads and grows below the gum line. Bacterial toxins and the body’s natural response to infection start to break down the bone and connective tissue that hold teeth in place. If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.
Do I have Gum Disease?
According to the American Dental Association, at least 60% of adults have moderate-to-severe gum disease! If you have any of the following symptoms you may have gum disease and should be checked by a dentist:
- Bad breath that won’t go away
- New spacing between teeth (caused by bone loss)
- Wiggly or loose teeth
- Sensitive teeth
- Swollen or red gums
- Tender or bleeding gums
- Feel pain when chewing
- Receding gums
Men are more likely to have gum disease than women. Although teenagers rarely develop periodontitis, they can develop gingivitis, the milder form of gum disease. Most commonly, gum disease develops when plaque is allowed to build up along and under the gum line. At your regular recall appointments and cleanings, we always evaluate the condition of your gums.
Treatment
Early treatment of gum disease is very important. The goals of treatment are to prevent gum disease from permanently damaging gum tissues, control infection, and prevent tooth loss.
Treatment for mild gum disease (Gingivitis)
If you have a milder type of gum disease (called gingivitis), you may be able to reverse the damage to your gums through regular brushing and flossing. You will need to come back for regular checkups and cleanings. Professional cleaning can remove plaque and tartar that brushing and flossing missed. After you have had gum disease, you may need to see your dentist every 3 or 4 months for follow-up. Your dentist may prescribe antibiotics to help fight the infection and recommend an antibacterial toothpaste that reduces plaque and gingivitis.
Treatment for advanced gum disease (Periodontitis)
Gingivitis that are not treated promptly or that do not respond to treatment can progress to advanced gum disease (called periodontitis). Periodontitis requires prompt treatment to get rid of the infection and stop damage to the teeth and gums, followed by long-term care to maintain the health of your mouth. Other treatment options include:
- Deep Cleaning (also known as Scaling and Root Planing) – Our registered dental hygienist will remove the plaque and tartar both above and below your gum line. Scaling means scraping off the tartar from above and below the gum line. Root planing gets rid of rough spots on the tooth root where the germs gather, and helps remove bacteria that contribute to the disease.
- Laser Dentistry – In some cases a laser may be used to remove plaque and tartar.
- Antibiotics – Your dentist may give you antibiotics to kill bacteria and stop the infection.
- Surgery – If these treatments don’t control the infection or if you already have severe damage to your gums or teeth a surgery may be required. Surgery options include:
- Gingivectomy – removal and reshaping of loose, diseased gum tissue to get rid of the pockets between the teeth and gums where plaque can build up.
- Flap procedure – cleans the roots of a tooth and repairs bone damage.
- Extraction – removes loose or severely damaged teeth
After treatment, you will need to keep your mouth disease-free by preventing plaque buildup. You will need to brush carefully and thoroughly after all meals and snacks and floss daily. Your dentist will schedule follow-up appointments regularly for cleaning and to make sure that the disease has not returned.

